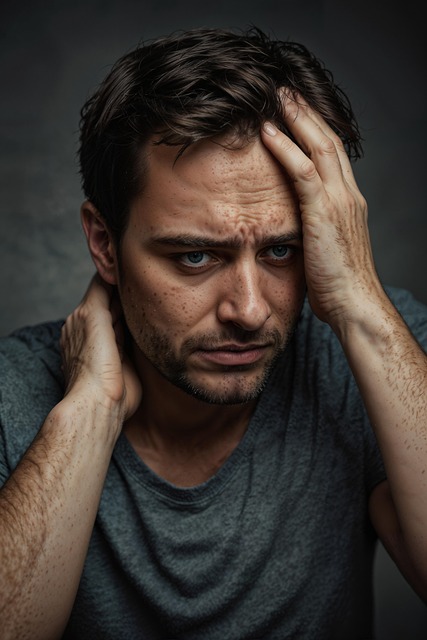
Diagnosing mental health conditions in older adults is complicated by age-related cognitive changes, physical comorbidities, historical trauma, and domestic violence. Depression in the elderly often manifests physically, while emotional regulation difficulties are linked to various conditions. Healthcare professionals need specialized training to address co-occurring disorders like domestic violence-related trauma, which requires tailored interventions for self-esteem improvement. The mental health crisis among elders is exacerbated by stigma, mobility issues, and financial constraints, necessitating tailored therapy, burnout prevention strategies, and stigma reduction initiatives. Effective solutions include therapy for elders and sensitive approaches to address domestic violence experiences to improve diagnosis and treatment outcomes.
Mental illness diagnosis accuracy among the elderly remains a complex challenge, with unique barriers such as stigma and cognitive changes hindering timely and effective interventions. This article explores innovative approaches designed to improve diagnostic accuracy, focusing on advanced assessment tools, therapy for elders, especially those facing domestic violence, and the integration of technology for remote mental health screening. Additionally, it highlights the critical roles of community outreach, education, and robust support systems in promoting early intervention and continuous care for better patient outcomes.
- Understanding the Challenges of Mental Illness Diagnosis in Elderly Populations
- – Prevalence of mental health issues among elders
- – Unique barriers to accurate diagnosis (e.g., stigma, cognitive changes)
Understanding the Challenges of Mental Illness Diagnosis in Elderly Populations

Diagnosing mental health conditions in the elderly can be a complex task due to several interconnected factors. As people age, they may experience cognitive changes, and comorbid physical health issues can often mask or complicate the presentation of mental illness. The unique challenges faced by older adults include potential age-related memory lapses, which might be mistaken for early signs of dementia instead of depression or anxiety. Furthermore, life experiences such as historical trauma or domestic violence, prevalent in many elderly individuals, can lead to complex emotional responses and behavioral changes, making diagnosis even more intricate.
The complexity is further amplified by the diverse range of symptoms that mental health disorders manifest in older populations. Depression, for instance, may present differently than in younger adults, with more physical symptoms like fatigue and sleep disturbances rather than persistent sadness or hopelessness. Similarly, emotional regulation difficulties can be a sign of various conditions, including those related to stress, trauma, or neurodegenerative diseases. Enhancing mental health awareness among healthcare professionals is crucial to overcoming these challenges, especially when considering co-occurring disorders, such as domestic violence-related trauma, which may require tailored therapy and support for self-esteem improvement in elderly individuals.
– Prevalence of mental health issues among elders

Mental health issues among elders are on the rise, with a significant portion of the aging population facing challenges like depression, anxiety, and even more severe conditions such as dementia. This demographic often faces unique barriers to accessing proper care due to societal stigma, limited mobility, and financial constraints. The impact of these issues is profound, affecting not only individuals’ quality of life but also their ability to maintain independence. According to recent studies, elder abuse, particularly domestic violence, contributes significantly to the mental health crisis in this age group, underlining the urgency for tailored interventions.
Addressing these concerns requires a multifaceted approach. Incorporating Mind Over Matter Principles into traditional therapy for elders can offer powerful tools for emotional regulation and coping mechanisms. Additionally, implementing Burnout Prevention Strategies for Healthcare Providers who specialize in elder care is crucial to ensuring consistent and compassionate support. By prioritizing mental wellness, we can create a safer, more supportive environment for elders, enabling them to lead fulfilling lives despite the challenges they face.
– Unique barriers to accurate diagnosis (e.g., stigma, cognitive changes)

Mental illness diagnosis can be hindered by several unique barriers, especially when it comes to elderly populations. One significant challenge is the stigma surrounding mental health issues, which often prevents individuals from seeking help or openly discussing their experiences. This reluctance can delay necessary interventions and support. Additionally, cognitive changes associated with aging may impact an elder’s ability to express or recall symptoms accurately, making diagnosis even more complex. These barriers highlight the need for tailored approaches in healthcare settings, particularly when addressing mental health concerns in older adults.
Addressing these issues requires a multifaceted strategy. For example, burnout prevention initiatives within healthcare professions can improve patient care and engagement. Developing mental wellness coaching programs specifically for elders can offer guidance and support while reducing the stigma associated with seeking help. Furthermore, mental illness stigma reduction efforts have a crucial role in creating an environment where individuals feel safe to discuss their mental health without fear of judgment, facilitating more accurate diagnoses and timely treatment, especially when considering the unique complexities faced by older adults exposed to therapy for elders or those who have experienced domestic violence.
Accurately diagnosing mental illness in elderly populations remains a complex task, exacerbated by age-related cognitive changes and the persistent stigma surrounding mental health. However, efforts to enhance diagnosis accuracy are pivotal for effective treatment, especially considering the heightened risk of conditions like depression and dementia among elders. Strategies such as comprehensive assessment tools and training in recognizing subtle symptoms can significantly improve outcomes. Furthermore, addressing domestic violence, a significant yet often overlooked factor, through specialized therapy for elders is crucial in providing holistic care and fostering mental well-being in this vulnerable demographic.